Description
Novel diagnostic for Parkinson’s disease
A new discovery at the University of Nebraska Medical Center could take most of the guesswork out of delivering an accurate and reliable diagnosis for Parkinson’s disease.
Current methods for diagnosing the more than 1 million Americans suffering from Parkinson’s involve a basic neurological exam and information provided by the patient. The resulting diagnosis in early stage patients is often inaccurate, inconsistent, and must be periodically reevaluated.
A team led by research physician Howard Gendelman—the 2008 Scientist Laureate, UNMC’s highest research honor—discovered a unique correlation between Parkinson’s disease and a protein found in a certain subset of immune cells called T-cells. An abundance of the protein could indicate a more severe case of the disease.
Researchers are currently developing a simple blood test that could help physicians detect and monitor the disease at the earliest stages. Early testing indicates a blood screen using this method would help patients and their doctors diagnose, track and monitor Parkinson’s disease with more accuracy and confidence than ever before.
To discuss licensing opportunities please contact Matt Boehm, PhD, at mboehm@unmc.edu or 402-536-9881.
Technical details
Methods for the diagnosis of Parkinson’s Disease
Researchers at UNMC have developed a novel approach for diagnosing and staging Parkinson’s Disease (PD) by measuring biomarkers found in patient blood samples. In addition, these methods could potentially be applied to a number of other neurodegenerative diseases such as Alzheimer’s Disease and amyotrophic lateral sclerosis.
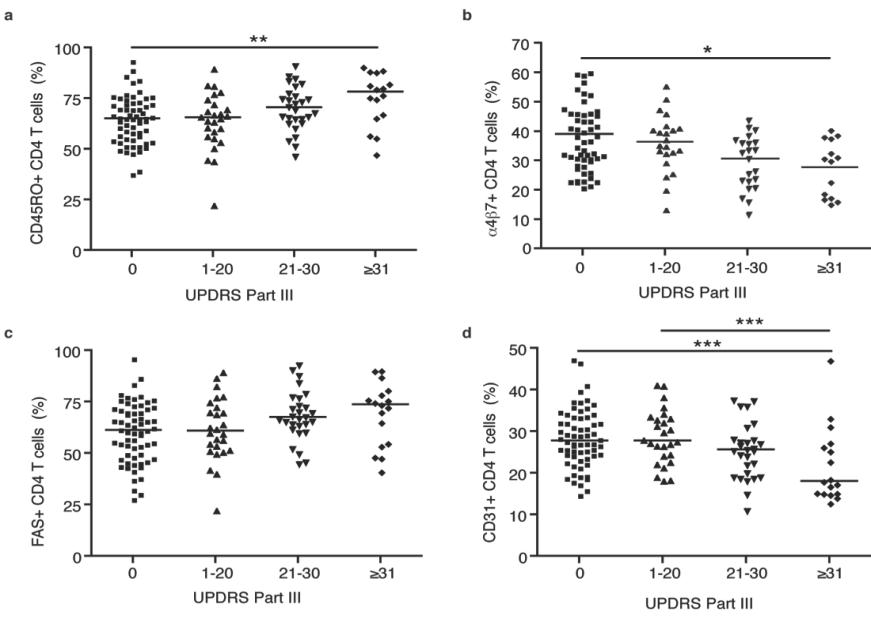
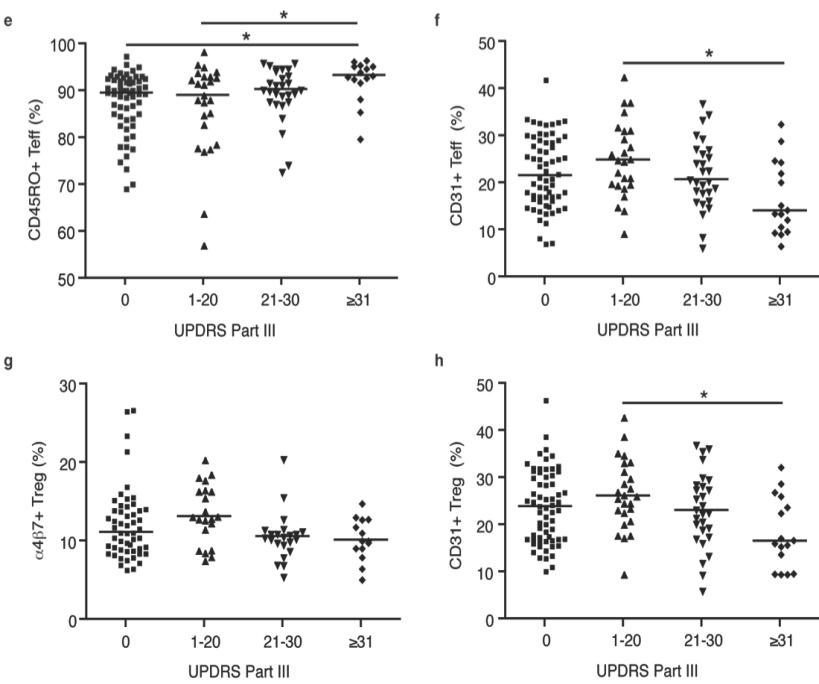
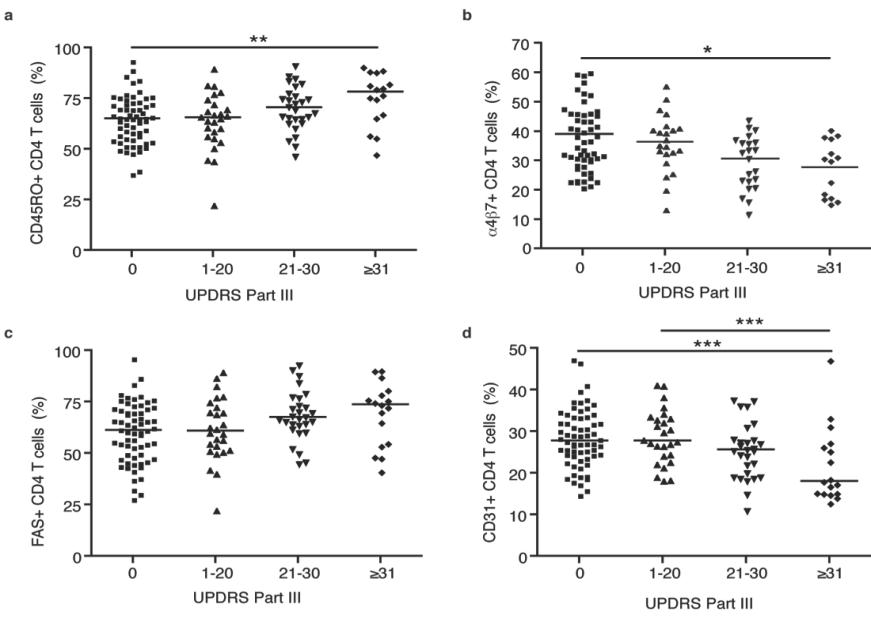
Here, markers are used for the detection and diagnosis of PD by comparing PD patient marker profiles with healthy individuals to uncover whether a given individual is affected, along with how severely, by measuring specific T cell populations and related cell surface markers. Through this method, UNMC researchers have conducted clinical studies demonstrating that PD patients have an increase in effector/memory T cells, a reduction in CD4+ T-cells and total lymphocytes, and a reduction in ITGΒ7 expression on CD4+ T-cells. These T-cell phenotypes were further correlated with PD using the United Parkinson’s Disease Rating Scale (UPDRS), which is the most commonly used scale for the clinical assessment of Parkinson’s (see below).
In addition to the T-cell phenotypes discovered, network analysis has revealed additional biomarkers that may be altered in PD and may be useful in the further development of this or related tests.